STS 2021, Day 2 — This year’s esteemed J. Maxwell Chamberlain Memorial Papers will compare the risk of complications and higher hospitalization costs in transcatheter versus surgical approaches to aortic stenosis (AS) and coronary artery disease (CAD), analyze the survival benefit of fundoplication for lung transplant recipients, examine the impact of medical center volume on readmissions and mortality following congenital cardiac surgery, and herald failure to rescue as a new STS quality metric for cardiac surgery. These top-scoring abstracts will be presented today during specialty-specific parallel sessions at 11:30 a.m. ET.

Nonsurgical Approaches to AS and CAD May Shorten Hospital Stays, but Increase Complications, Costs
While surgical aortic valve replacement (AVR) with coronary artery bypass grafting (AVR+CABG) is the recommended treatment for AS and CAD, heart teams are increasingly opting for less-invasive percutaneous coronary intervention (PCI) at the time of transcatheter aortic valve replacement (PCI+TAVR). During his Chamberlain Paper for Adult Cardiac Surgery presentation, Sri Harsha Patlolla, MBBS, from the Mayo Clinic in Rochester, Minnesota, will compare outcomes of these two approaches in a National Inpatient Sample cohort from 2012 to 2017.
While Dr. Patlolla’s team found that in-hospital mortality was comparable in the AVR+CABG and PCI+TAVR groups, they discovered that, despite shortening hospital stays by a day, PCI+TAVR was associated with higher complication rates—including a greater need for pacemaker implantation, higher rates of cardiac arrest, and more vascular complications—and higher hospitalization costs.
After Dr. Patlolla’s presentation, discussant Michael J. Reardon, MD, from Houston Methodist DeBakey Heart & Vascular Center in Texas, will discuss the research and implications of the findings.

Mortality Rates Decrease Significantly for Congenital Cardiac Operations at High-Volume Hospitals
Increased congenital cardiac surgery volume is associated with improved mortality, reduced duration of hospitalization, and fewer readmissions within 30 days, according to research from the Chamberlain Paper for Congenital Heart Surgery.
Catherine G. Williamson, a medical student at the University of California, Los Angeles, will present data from the Nationwide Readmissions Database (2010 to 2017) that demonstrate the positive impact of hospital volume on outcomes beyond acute hospitalization.
After adjustment, an incremental increase of 50 annual congenital heart disease cases was associated with a 26% reduction in mortality, a 16% decrease in non-home discharge, and a 4% reduction in 30-day non-elective readmission, said Williamson.
Despite concerns about the use of advanced resources at expert centers, the results showed lower 30-day costs if care was delivered at a high-volume hospital. The findings may have implications for the centralization of care and quality outcomes in patients with congenital heart disease. Therefore, said Williamson, policy and insurance-based reform is both necessary and advantageous to ensure that patients have equal access to care at expert centers.
Scott M. Bradley, MD, from the Medical University of South Carolina in Mount Pleasant, will serve as discussant for this paper.
Findings Identify Lung Transplant Recipients Who Benefit Most from Fundoplication
Lung transplant recipients who undergo fundoplication exhibit improved long-term survival and a decreased rate of chronic lung allograft dysfunction (CLAD) related to gastroesophageal reflux and aspiration. Chamberlain Paper for General Thoracic Surgery presenting author Miguel M. Leiva-Juarez, MD, a research fellow at Columbia University Medical Center in New York, New York, will discuss findings from a 20-year retrospective study that sought to identify recipient populations who can achieve the most survival benefit from fundoplication.
Fundoplication, both before and after the occurrence of CLAD, was shown to be an independent predictor of survival, said Dr. Leiva-Juarez. When patients received fundoplication before development of CLAD, they tended to experience improved overall survival, while patients receiving fundoplication after developing CLAD had an increase in post-CLAD survival compared with patients who didn’t undergo fundoplication.
The procedure was most beneficial for recipients under the age of 65 years and those with restrictive disorders, and the benefit was independent of the type of transplant. A diagnosis of gastroesophageal reflux by conventional methods was not a significant predictor of survival, Dr. Leiva-Juarez noted.
Errol L. Bush, MD, from Johns Hopkins Medicine in Baltimore, Maryland, will discuss this paper.
Failure to Rescue Emerges as New STS Quality Metric for Cardiac Surgery
In the earliest planning stages of the STS National Database, the founders recognized the importance of risk adjustment—but they also acknowledged that measurement of professional performance isn’t just about mortality rates, said author Paul Kurlansky, MD, from Columbia University Medical Center in New York, New York, who will present the first-ever Chamberlain Paper for Perioperative and Critical Care.
Dr. Kurlansky and colleagues studied failure to rescue as a risk-adjusted metric in 1,128 patients from the STS Adult Cardiac Surgery Database, including patients who underwent isolated CABG, AVR with or without CABG, or mitral valve repair/replacement with or without CABG between January 2015 and June 2019.
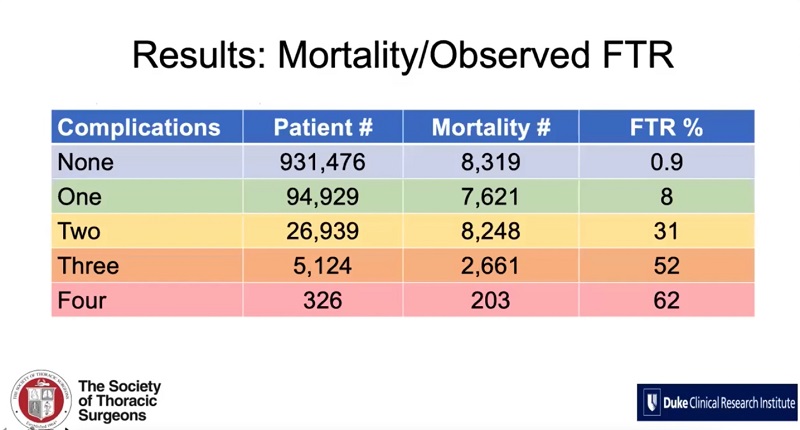
This new failure to rescue metric complements existing STS performance measures and specifically assesses institutional effectiveness of postoperative care. This will allow hospitals to develop targeted quality improvement efforts. Incorporation of the metric also may provide valuable information that can be used in patient and family counseling when discussing the likelihood of survival after postoperative complications, Dr. Kurlansky said.
Glenn J.R. Whitman, MD, of The Johns Hopkins Hospital in Baltimore, Maryland, will discuss this Chamberlain paper.
Read more Daily Bulletin stories.