STS News, the Society’s quarterly magazine for members only, brings you the latest CT surgery news, research, advocacy updates, surgeon stories, and more to help keep you in the know and connected to your peers. Read it today.
STS News Archives:
Top Story
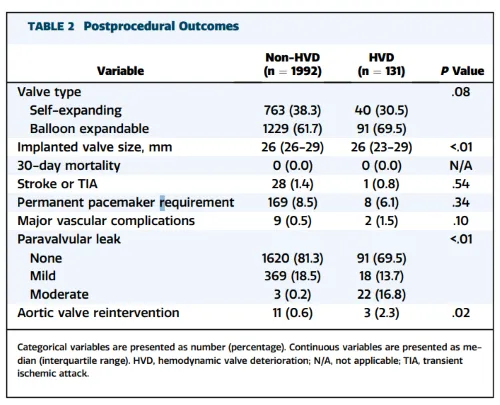
New Study Identifies Early Signs of Valve Failure One Year After TAVI, Raising Durability Concerns in Younger Patients
A new study published in The Annals of Thoracic Surgery, a journal from The Society of Thoracic Surgeons, has identified early hemodynamic valve deterioration (HVD) in more than 6% of patients just one year after undergoing transcatheter aortic valve implantation (TAVI).
Read how this raises new questions about valve durability in younger, lower-risk populations.
Latest news
Browse news by topic

Member News
Learn about member experiences from your specialty, and stories about the ever-evolving landscape of cardiothoracic surgery.

Technology
Learn about science, technology, and date-driven tools made possible by the STS National Database.

Advocacy
Learn about Leadership, Advocacy, and Regulatory Action; you and your colleagues are taking steps to drive change in healthcare institutions and on Capitol Hill.
The STS Blog
From career advice to expert perspectives illuminating the latest findings in the media, STS authors share their insights and experience.
Press Releases
News and announcements for cardiothoracic surgery, the health care press, and the public.
For Media Representatives
All media inquiries, including requests for interviews with leading experts in cardiothoracic surgery.
Share your news and stories
STS wants to hear from its members and share their news and stories with others. Working on new research or an innovative initiative? Making an exciting career move? Receiving a promotion? Honored with an industry award? Send us an email at stsnews@sts.org.