When a patient who has undergone a cardiac surgery procedure begins to decline postoperatively, there’s often a narrow window in which early recognition and rapid, coordinated response can mean the difference between recovery and catastrophe.

For Rakesh Arora, MD, the director of perioperative and cardiac critical care at University Hospitals Harrington Heart & Vascular Institute, and clinical professor at Case Western Reserve University School of Medicine, that window is where team structure and communication protocols either hold or break.
“There's a spectrum of cardiac emergencies,” said Dr. Arora. “Some are the slowly slipping patients, gradually declining, not following the recovery path. And then there are unanticipated catastrophes, like cardiac arrest, where you need a team that's trained to respond immediately.”
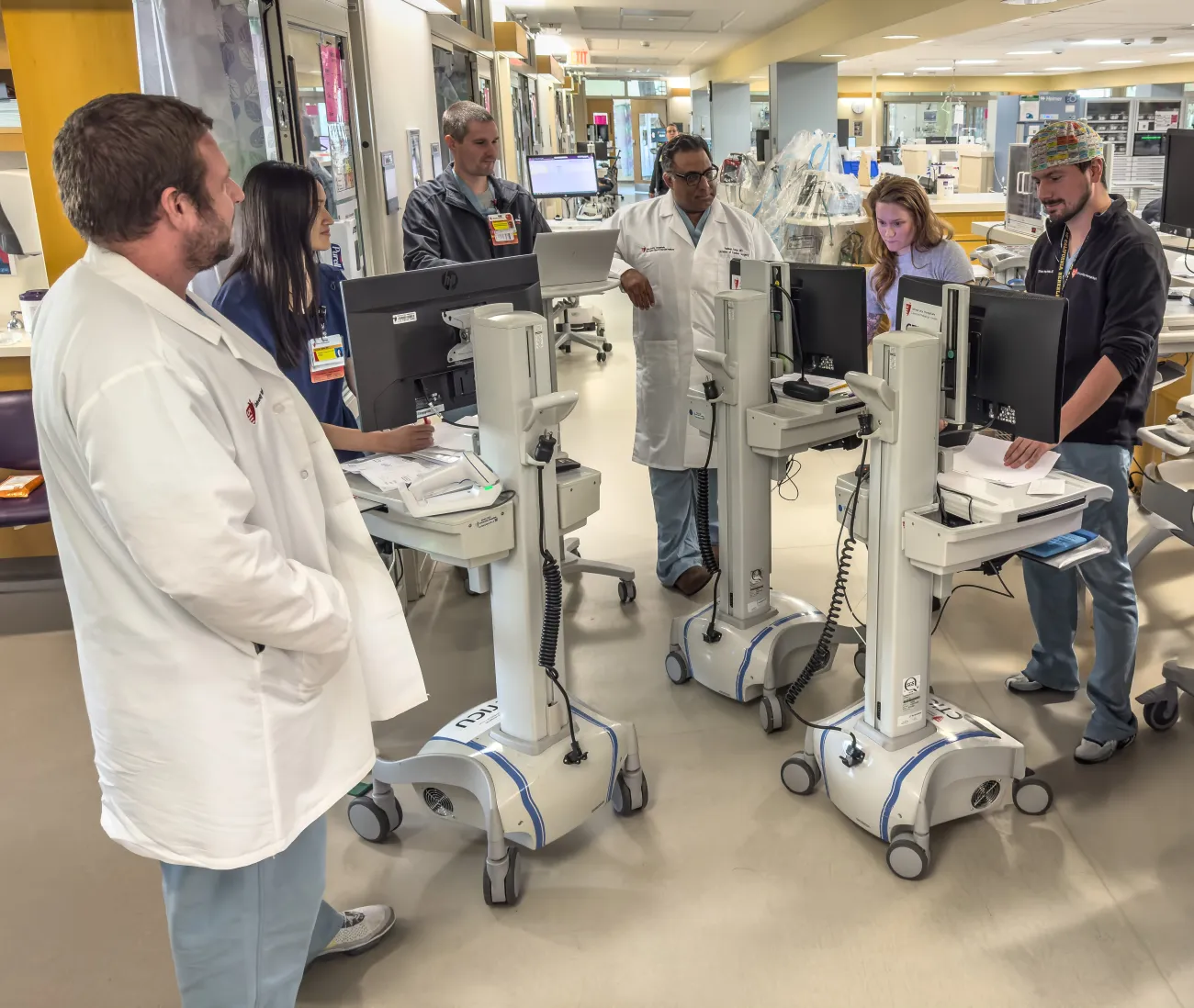
Over the past three years, Dr. Arora and the perioperative team at UH Harrington Heart & Vascular Institute have sought to develop and implement innovative, scalable team models designed to enhance outcomes during high-stakes moments. His approach integrates clear care pathways, interdisciplinary communication protocols, and continuous data review — all aimed at identifying issues early and coordinating an effective response.
Here, he shares the team's seven strategies for creating, scaling, and sustaining high-functioning, multidisciplinary teams.
1. Start with the "Why" and Make It Universal
“Everyone comes with their perspective on what’s best for the patient,” Dr. Arora says. “The ICU clinician, the surgeon, the pre-op coordinator, they may each define success differently.”
Establishing a shared purpose among all stakeholders is essential. Dr. Arora recommends engaging key team members early in the design process to align goals, build trust, and create a culture of collaboration. A clearly defined “why” helps teams stay grounded when protocols evolve or crises emerge.
“Ask the team: Why are we doing this? Everyone wants what’s best for the patient, but what that looks like can vary depending on your role. You have to bring those perspectives together,” added Dr. Arora.
2. Standardize Pathways, But Build in Flexibility
At Dr. Arora’s main hospital site, every patient follows a structured care path that begins the moment they enter the ICU after surgery. These protocols detail expected milestones from minute zero to hour 24, including escalation triggers for when patients deviate from their recovery track.
But one size doesn’t fit all. Community sites with different resources and volume of cases require adaptations. “We had to create systems that work both at our downtown center and at lower-volume sites,” says Dr. Arora. Flexibility ensures standardization doesn’t come at the cost of ignoring local clinical context.
3. Empower Anyone to Trigger Escalation
“You can’t overcommunicate,” says Dr. Arora. In their model, bedside nurses, residents, APPs, and physicians are all empowered to escalate care concerns. If a patient isn’t meeting their milestones, that deviation serves as a trigger to alert the next level of providers, starting with frontline staff and escalating to intensivists and surgeons as necessary. For patients experiencing cardiogenic shock, a dedicated “shock call” system ensures a multispecialty team is promptly activated.

“Our shock team is available by phone 24/7 and must respond within 15 minutes,” says Arora. “It includes a cardiac surgeon, the CTICU intensivist, CICU attending, interventional cardiologist, and the referring clinician.” Together, they develop a transport and escalation plan, re-engaging the team upon the patient’s arrival if further intervention is needed, such as mechanical circulatory support.
This system-wide response framework helps community hospitals, where volumes may be lower and resources more limited, get immediate access to the expertise and equipment concentrated at the downtown hub.
4. Build Communication into the Culture
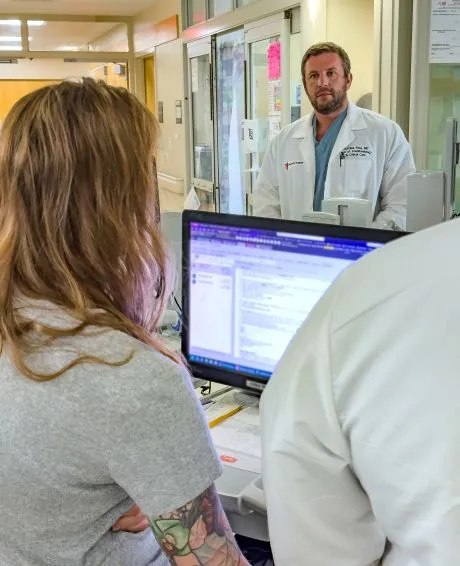
Sustained team performance requires more than protocols. It takes “spot checks,” data reviews, and constant reinforcement. Dr. Arora regularly visits various ICU sites to monitor implementation, ensure accurate documentation, and maintain fidelity to care pathways.
“Communication is still a work in progress,” he admits, but the cultural expectation is clear: speak up early and often. “If something doesn’t smell right,” he says, “someone needs to say something.”
5. Data, Dashboards, and Measuring What Matters
While real-time dashboards are the goal, Dr. Arora’s team currently uses audit tools and regular quality improvement meetings to assess performance. Cases that fall outside the care pathway or result in preventable complications are reviewed at both the local and system levels.
“When something goes wrong, we do a deep dive to determine where there are opportunities to improve our processes. Was it a communication issue? Was there a failure to recognize deterioration?” says Arora. “Then we implement changes, such as redundancies, safeguards, and retraining.”
To measure progress, Dr. Arora’s teams track performance across four domains: adherence to enhanced recovery protocols, postoperative complication rates, length of stay, and readmissions. These metrics are tied to the STS National Database, as well as internal dashboards.
One key performance indicator, for instance, is achieving 80% adherence to enhanced recovery after surgery (ERAS) protocols. Others include achieving three-star STS ratings across key complications, such as prolonged ventilation, stroke, and renal failure. Dr. Arora’s center has recently achieved this distinction for their coronary artery bypass patients.
“We’ve also added ICU bounce-back rates and hospital readmissions to our system dashboards,” Arora says. “The data helps us have team-based conversations around patient-centered outcomes.”
6. Innovate with Technology, But Know Its Limits
Dr. Arora sees real promise in AI-driven predictive models that alert care teams to patient deterioration before it becomes obvious.
“There are systems that are pulling real-time hemodynamic data and displaying color-coded risk,” he says. While promising, many are costly and not yet widely scalable. Still, he believes these tools will increasingly help clinicians “recognize when something isn’t right before it becomes a crisis.”
He’s particularly excited about technologies that integrate real-time data with AI to predict deterioration before it’s clinically obvious. “It’s moving us [slowly] towards Minority Report,” he says, referencing the film where crimes are predicted before they happen. “We’re talking about streaming data, multiple data points per second, and using machine learning to give us early warning signs. That’s the future.”
7. Think Synergy, Sustainability, and Scalability
For surgeon-leaders looking to replicate this model, Dr. Arora offers three pillars:
• Synergy: Engage stakeholders across roles and locations.
• Sustainability: Avoid burnout by designing systems that last.
• Scalability: Tailor solutions to each site’s needs while staying anchored to core goals.
“Some days it feels a little like building the plane while you’re flying it,” he says. “Each site has different resources and cultures. You have to respect that while still delivering the same standard of care.”
Reinvention Is Part of the Process
Having previously built a similar system at an institution in Canada, Dr. Arora knows firsthand that success doesn’t always transfer cleanly. “What got me here isn’t going to get me there,” he says. “Every project and every team require reinvention.”
His advice? Meet people where they are, aim for early wins, and always start with why.
