Discover the featured content in this month’s The Annals of Thoracic Surgery issue, personally selected by Editor-in-Chief Dr. Joanna Chikwe & Senior Editor Dr. Robbin Cohen, who highlight the authors' important findings, with select illustrations from Dr. Sarah Chen, Associate Editor/CMI. As an additional benefit to your STS Membership and Annals subscription, this monthly newsletter aims to bring expert perspectives on recently published research, straight to your digital doorstep.
Featured in the February 2026 issue...
Global Health | Redefining Success in Cardiac Surgery in Africa: Aligning Training, Patient Profiles, and Outcomes
Manuel, Salmane Ba, and coauthors
This article proposes a critical reassessment of what “success” truly means in the context of cardiac surgery in Africa. The authors advocate for evaluation criteria that reflect local epidemiologic realities, given the dual challenges of adapting advanced surgical techniques to a complex patient population and the need for tailored risk tools that accurately predict outcomes in resource-constrained settings.
-Joanna Chikwe, MD
Editor-in-Chief
Valve | Early Hemodynamic Valve Deterioration After Transcatheter Aortic Valve Implantation
Ashwat, Sultan, and coauthors
In this single-center analysis of 4317 patients who underwent transcatheter aortic valve replacement between 2012 and 2022, of whom 2123 (49%) had 1-year echocardiographic follow-up, 131 (6.2%) exhibited echocardiographic evidence of hemodynamic valve deterioration (defined as an increase in mean transvalvular gradient ≥10 mm Hg resulting in a mean gradient >20 mm Hg or an increase of ≥1 grade of intraprosthetic aortic regurgitation resulting in ≥ moderate aortic regurgitation). Such patients were significantly younger and more likely to have smaller aortic annuli (23 mm vs 24 mm; P < .01) compared with patients without hemodynamic deterioration at one year.
-Joanna Chikwe, MD
Editor-in-Chief
Valve | Exercise in Patients With Bicuspid Aortic Valve and Aortic Dilation
Saleh, Puthumana, and coauthors
In a prospective cohort study of 566 patients undergoing longitudinal cross-sectional imaging surveillance for bicuspid aortic valves and ascending aortic dilation >4.0cm for a median of 8 years, vigorous exercise was not associated with progressive aortic dilation, and there were no instances of acute aortic syndrome.
-Joanna Chikwe, MD
Editor-in-Chief
Lung | Segmentectomy vs Lobectomy for Occult N1 in Non-Small Cell Lung Cancer: Is Less More?
Abdallat, Wiener, and coauthors
In 185 patients with occult N1 non-small cell lung cancer, 30 (16.2%) underwent segmentectomy and 155 (83.8%) underwent lobectomy. Patients undergoing lobectomy had larger pathologic tumor sizes than those undergoing segmentectomy (3.4 cm [interquartile range, 2.30-4.45 cm] vs 1.95 cm [interquartile range, 1.43-2.83 cm], P < .005), and similar rates of adjuvant (67% vs 70%, P = .7), respectively. There were no significant differences in 5-year survival or locoregional recurrence-free survival between segmentectomy and lobectomy.
-Joanna Chikwe, MD
Editor-in-Chief
Transplant & Mechanical Support | National Outcomes of Nonintubated Extracorporeal Membrane Oxygenation as a Bridge to Heart Transplantation
Akbar, Kilic, and coauthors
In an analysis of the United Network for Organ Sharing database, 857 heart transplant recipients were bridged to transplant with extra corporeal membrane oxygenation (ECMO) between 2018 and 2023. Extubating patients on ECMO was associated with better peritransplant outcomes, including lower risk of stroke and dialysis, and better short- and long-term survival after transplant compared with continuing mechanical ventilation on ECMO.
-Joanna Chikwe, MD
Editor-in-Chief
Education & Professional Development | Parenthood and Family Building Challenges Among Cardiothoracic Surgery Trainees
Lopez, Watkins, and coauthors
Approximately 20% of 454 cardiothoracic surgery trainees responding to the 2024 Thoracic Surgery Directors Association In-Training Exam survey were either pregnant or had a pregnant partner during their cardiothoracic surgery training. Barriers to family planning, parenthood, parental leave, perinatal care, and breastfeeding persist. Policies and implementation of these policies are needed to support parenthood and family planning among CT surgery trainees.
-Joanna Chikwe, MD
Editor-in-Chief
Education & Professional Development | Defining the Learning Curve in Minimally Invasive Cardiac Surgery: A Systematic Review and Meta-Analysis
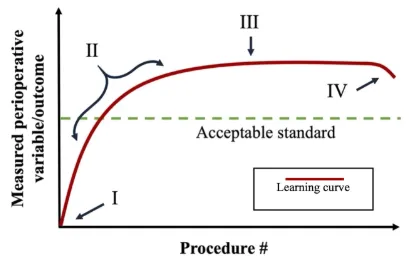
Elsebaie, El-Diasty, and coauthors
This meta-analysis explored 28 previously published studies to better define the learning curve for non-robotic minimally invasive aortic valve, mitral valve, and coronary artery bypass procedures. The number of procedures suggested to overcome the learning curve ranged between 23 and 125, with 75-100 cases being the most frequently reported thresholds. The authors discuss the impact of interprocedural differences, surgeon experience, and program volume on learning curve and surgical outcomes.
-Robbin Cohen, MD, MMM
Senior Editor
Coronary | Arterial Grafting Survival Benefit in End Stage Renal Disease Patients Undergoing Coronary Arterial Bypass Grafting
Yang, Kurlansky, and coauthors
The United States Renal Data System was used to compare LIMA plus SVG (89.8%), SVG only (7.1%), and multiarterial (MAG) grafting (3.1%) in end stage renal failure patients who underwent isolated CABG from 2015-2021. Of 16,616 patients who underwent CABG, 1190 underwent subsequent renal transplantation. LIMA showed a 5-year survival benefit compared with SVG only in patients not receiving transplants (31.6% vs 26.6%; p <.001), though this difference diminished after 4 years. There was no survival benefit with MAG over LIMA regardless of subsequent transplantation status. In their invited commentary, Ahmed Awad and Faisal Bakaeen discuss the limited survival of end-stage renal disease patients on dialysis, and the complexities associated with evaluating conduit choices in this challenging cohort.
-Robbin Cohen, MD, MMM
Senior Editor
Lung | Lung Transplantation in the Elderly: Is Age a Contraindication?
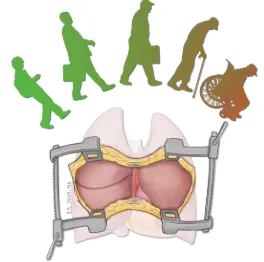
Shacker, Smith, and coauthors
The results of bilateral lung transplantation in 970 patients were analyzed according to age in this single institution report. Study groups included ages 15-64 yrs (49.5%), 65-69 yrs (28.6%), 70-74 yrs (19.7%), and 75-79 yrs (2.3%), with an increasing trend toward older patients over time. Older patients had a higher rate of male sex, white race, and restrictive lung disease (P<.001). They had longer lengths of stay, but rates of posttransplant dialysis, stroke, and prolonged ventilatory support were similar between groups. Though survival rates were the highest in the 15-64 yrs age group (58%), the older age groups had 5 year survival rates of 46.8% (65-69 yrs), 44.5% (70-74 yrs), and 47.2% (75-79 yrs). In his invited commentary, Trevor Ellison acknowledges the success of lung transplantation in the elderly, but challenges the trend toward their allocation given current donor restraints.
-Robbin Cohen, MD, MMM
Senior Editor