Lung cancer screening has been proven to save lives, yet participation rates remain alarmingly low. The National Lung Screening Trial (NLST) conducted in the US demonstrated that low-dose CT screening significantly reduces lung cancer mortality, but only 16.5%-18% of eligible individuals undergo recommended screenings.
This gap in participation is particularly concerning given the stark contrast in survival rates: the latest studies show that early detection leads to an 80% survival rate at 20 years, while late-stage diagnoses translate to a five-year survival rate of just 8%.
Barriers to screening include a lack of awareness about lung cancer risk factors and screening benefits, financial constraints, geographic limitations, and insufficient political prioritization of lung cancer prevention. Addressing these obstacles is critical to improving outcomes.
The Science Behind Limited Access and Eligibility
Underserved populations not only have inadequate access to information on the risks of lung cancer and the benefits of screenings, they also have limited access to healthcare facilities. According to a study led by Rian M. Hasson, MD, thoracic surgeon and vice chair for Workforce Development and Engagement, Brigham and Women’s Hospital, lung cancer rates are notably higher in rural and low-income regions, with 215 cases per 100,000 men in the poorest areas compared to 94 cases in affluent areas. The study concludes that “improving equitable access to high-quality screening services in rural regions and creating targeted interventions to address decreased access in areas of high tobacco use and low education is vital to decreasing the incidence of late-stage presentations of lung cancer in these populations.”
Strict eligibility criteria are a barrier to lung cancer screening for high-risk individuals. The US Preventive Services Task Force (USPSTF) recommends screening only for those aged 50 to 80 with a 20-pack-year smoking history who currently smoke or quit within the past 15 years. Because these guidelines determine insurance coverage, those who don’t qualify may face out-of-pocket costs ranging from hundreds to thousands of dollars.
A new study by Alexandra Potter, a researcher at Massachusetts General Hospital and president of the American Lung Cancer Screening Initiative, and Chi-Fu Jeffrey Yang, MD, a thoracic surgeon at Massachusetts General Hospital, investigated how well current lung cancer screening guidelines identify high-risk individuals.
The paper, selected as the J. Maxwell Chamberlain Memorial Award Paper in General Thoracic Surgery at STS 2025, analyzed data from 7,186 patients diagnosed with lung cancer, making it the largest study of its kind to date. The findings revealed that only 46.1% of patients diagnosed with lung cancer would have met the current 2021 USPSTF criteria. More than half of those diagnosed with lung cancer would not have qualified for screening.
The study evaluated whether alternative screening guidelines would identify more people with lung cancer. Replacing the USPSTF’s 20-pack-year smoking requirement with a 20-year smoking duration increased eligibility from 46% to 49%, expanding access for younger individuals, women, and racial and ethnic minorities. Under the American Cancer Society guideline—which removes the 15-year quit-time limit—eligibility among former smokers rose from 36% to 65%. The National Comprehensive Cancer Network’s updated 2024 guideline, which recommends screening for anyone 50 and older with a 20-pack-year history regardless of quit date, identified the highest proportion of cases—72%.
"Our study highlights a critical gap in current lung cancer screening eligibility criteria,” said Potter. “Removing the 15-year-since-quitting requirement could substantially expand access to lung cancer screening for more individuals who formerly smoked and are at high risk for lung cancer.”
Yang emphasized, “These findings have important implications for improving eligibility criteria for lung cancer screening to include more people at high risk of developing the disease. Our hope is that these findings can be taken into consideration during the next round of revisions to the USPSTF lung cancer screening recommendation.”
The Role of Mobile Screening Programs
Expanding lung cancer screening eligibility is one way to improve participation rates. Another is the expansion of mobile lung cancer screening programs.
Mobile LCS units bring screening services directly to people living in healthcare deserts. These mobile initiatives generally target high-risk populations with a history of smoking and who fall within a specific age range: 50 to 80 years old with a significant smoking history, such as a 20-pack-year. And they are making a measurable difference.
A recent study analyzed 12 research articles published between 2017 and 2023, documenting 10 mobile low-dose computed tomography (LDCT) programs worldwide. These platforms primarily served high-risk populations, including smokers, individuals in rural areas, and uninsured or underinsured patients.
Reported lung cancer diagnoses from these platforms ranged from 0.33% to 3%, with the majority (80%) of detected cases at stages I and II. The study underscores mobile LDCT platforms as a “powerful solution to enhance access to LCS, especially for marginalized populations” and that “by improving screening rates and enabling early detection, these platforms hold promise in narrowing healthcare disparities.”
Breathe Easy Program: A Game-Changing Mobile LCS Initiative

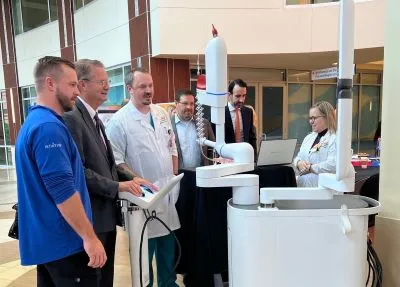
Robert Headrick, MD, chief of thoracic surgery, CHI Memorial, spearheaded a transformative mobile LCS initiative to improve early lung cancer detection and patient outcomes. Launched in 2018, the Breathe Easy program takes a proactive, community-centered approach to identifying high-risk individuals and ensuring they receive timely screenings and care.
By breaking down barriers such as geographic access, socioeconomic limitations, and patient hesitancy, Breathe Easy is helping to close critical gaps in lung cancer care. The initiative leverages mobile screening units, partnerships with primary care providers, and educational campaigns to increase awareness and encourage at-risk populations to seek screening. Patients who test positive for lung nodules or early-stage cancer can swiftly receive follow-up care.
Since its inception, Breathe Easy has reached more than 11,000 people who would not have known about lung screening or had access to a screening center. The majority of cancers found (80%) are in early stages. Compliance with annual screening has been 70%, attributed to the convenience of the 7-minute visit, which respects the patient’s time.
The program also includes a coronary artery calcium score with each scan. It has helped those with asymptomatic coronary artery disease get on statin therapy, reducing their risk for myocardial infarction. These outcomes highlight the program’s effectiveness in identifying lung cancer and now also coronary artery disease at its most treatable stages, ultimately improving patient survival rates and quality of life.
Beyond patient statistics, the program has fostered strong collaborations between healthcare institutions, local organizations, and public health agencies, strengthening the collective fight against lung cancer.
“As surgeons, we are problem solvers,” said Dr. Headrick. “But this problem requires more than just our surgical skills. It requires us to look outside our four walls to collaborate and find new concepts that give people easy access to healthcare.”
Mobile LSC Deployment

Deploying a mobile LCS program presents complex challenges, including financial constraints, logistical hurdles, and cultural barriers, all of which can hinder widespread adoption.
One of the most significant obstacles is funding. The high cost of mobile units, staffing, and ongoing operations can be prohibitive. Without consistent funding streams or reimbursement for screening services, program expansion remains difficult. Hidden ancillary costs—such as patient transportation and follow-up care—further complicate long-term sustainability.
Infrastructure and technology pose additional challenges. Mobile units require reliable power sources, secure storage for equipment, and specialized technology to perform screenings. Maintaining these resources demands skilled personnel, who can be difficult to secure in areas already facing workforce shortages.
Education and awareness are equally critical. Many patients and even healthcare providers remain unaware of lung cancer screening guidelines and eligibility criteria. In some communities, cultural stigmas surrounding smoking and lung cancer discourages individuals from seeking screening, reinforcing disparities in early detection.
A Holistic Approach to Implementation
Successfully developing and deploying mobile LCS initiatives requires collaboration among healthcare organizations, community leaders, and policymakers. A coordinated effort is essential to ensure mobile screening programs are accessible and sustainable. It starts with the formation of a multidisciplinary team.
Pulmonologists and radiologists play a central role in interpreting LDCT scans and ensuring that patients receive appropriate follow-up care. Primary care physicians help identify and refer high-risk individuals, particularly those with a history of smoking. Meanwhile, healthcare administrators coordinate staffing, technology, and data management to seamlessly integrate screening programs into existing healthcare infrastructure.
Beyond Medicine: Community Engagement
Community leaders play a vital role in improving public health and expanding access to mobile LCS. Local organizations—such as faith-based groups and social service agencies—can help raise awareness, build trust, and reach high-risk populations. Yet, as Dr. Headrick emphasizes, it is often lung cancer survivors themselves who drive the most meaningful change.
“The real game-changers in getting mobile LCS programs up and running are lung cancer survivors who share their stories,” said Dr. Headrick. “It’s the cancer patient stories that show us why lung cancer screening initiatives matter.”
He added, "Survivors are the ones who can go into the community and deliver messages about early detection that resonate. They are the reason more people choose to get screened."
Advocating for Lung Cancer Screenings
As leaders in lung cancer care, thoracic surgeons can help ensure more people receive the screenings they need to detect lung cancer early and improve survival by participating in healthcare policy-making processes.
During the last session of Congress, Representatives Larry Bucshon, MD (R-IN), Raul Ruiz, MD (D-CA), Vern Buchanan (R-FL), and Debbie Wasserman Schultz (D-FL) introduced bipartisan legislation, supported by STS members, to improve patient access to cancer screenings. The bill would create a competitive grant program within the Health Resources and Services Administration (HRSA) to fund mobile cancer screening units, with a focus on lung cancer. Grants of up to $2 million would help cover the cost of vehicles, LDCT scanners, and necessary software.
The UT Medical Center in Knoxville received a $5.46 million grant from the State Department of Health to support its mobile lung cancer screening program. STS submitted a letter backing the funding request.
STS members can advocate for policies supporting lung cancer screening by:
- Engaging with policymakers to secure funding and support for screening initiatives.
- Emphasizing the need for comprehensive screening programs and equitable access.
- Encouraging members to support policies that aid lung cancer patients and allocate federal funding for screening programs.
- Urging members to contribute to the STS-PAC fund, which helps make these efforts possible.
Looking Ahead
Success in mobile LCS programs is measured not only by the number of screenings performed but also by the program’s ability to detect cancer early, improve patient outcomes, and reduce healthcare disparities. As mobile LCS programs expand, defining clear benchmarks for effectiveness will be necessary to ensure long-term impact and sustainability nationwide. Ongoing evaluation and adaptation will be key to maximizing the impact of these programs on public health.
Learn more about mobile lung cancer screening programs and check out the STS Roadmap to Lung Cancer Screening toolkit for step-by-step information on developing or expanding mobile lung cancer screening programs.
