STS News, Summer 2020 — The COVID-19 global pandemic has pushed many medical specialties to the limits—health care professionals working around the clock taking care of the sickest of patients, putting their lives on the line like never before, and struggling to handle growing patient loads and death rates, often with limited resources.
Cardiothoracic surgery has been no exception.
In many ways, cardiothoracic surgeons—who are comfortable in high-pressure, intensely demanding situations—were made for times like these.
“I think this is a good place for cardiothoracic surgeons to be,” said Brendon M. Stiles, MD, from NewYork-Presbyterian/Weill Cornell Medical Center in New York. “We certainly do not want to be sitting at our desks in our offices while others do the work.”
Vinod H. Thourani, MD, from Piedmont Heart Institute in Atlanta, Georgia, echoed that sentiment. “We were born for this type of intense work since we have extensive training in critical care, cardiac surgery, and cardiopulmonary physiology,” he said.
Cardiothoracic surgeons are uniquely equipped to handle the arduous work involved with fighting a global health emergency. John S. Ikonomidis, MD, PhD, from the University of North Carolina at Chapel Hill, explained that heart and lung surgeons—with their formidable personalities and strong opinions—are comfortable in the role of “captain of the ship.”
“Over years of training, we have developed the stamina and focus that enables us to get through long and stressful days and still be able to come back for more,” he said.
Few career paths offer the same personal and professional satisfaction as that of a cardiothoracic surgeon. This is where “medicine best embodies the interface between humanity and science,” Dr. Ikonomidis said, making cardiothoracic surgery “one of the most rewarding specialties to choose.”
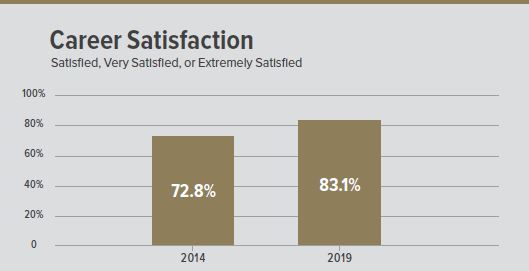
An increasing number of cardiothoracic surgeons agree, according to the 2019 STS Practice Survey. This workforce survey—carried out approximately every 5 years since the early 1970s—helps establish a current, detailed profile of the specialty. The results showed that 83.1% of surgeons are either satisfied, very satisfied, or extremely satisfied with their current career, compared with 72.8% in 2014.
In addition, half of practicing surgeons would recommend that their children or grandchildren pursue a career in cardiothoracic surgery, while only 47.5% and 37.1% reported feeling that way in 2014 and 2009, respectively. Some surgeons are even postponing retirement because they have a “high level of career satisfaction.”
“When a surgeon heals a patient through a carefully thought-out and expertly performed procedure followed by compassionate and comprehensive postoperative care, a deeply satisfied feeling ensues, which never dulls with time or age,” said Dr. Ikonomidis.
Even so, these are trying times for the specialty.
The training to become a cardiothoracic surgeon has been criticized for being too rigorous and lengthy, the educational debt tremendous, and the workloads and work hours too excessive and stressful.
The survey showed that 68.9% of surgeons had 7, 8, or 9 years of training (21.8%, 25.0%, and 22.1%, respectively), while 29.2% reported having 10 years of post-MD training prior to entering practice.
At the same time, the educational debt accumulated by these surgeons is staggering, with 17.8% having $150,000 or more at the time they began active surgical practice.
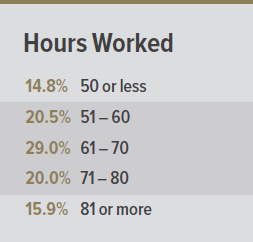
The long and irregular hours often worked by cardiothoracic surgeons may impact wellbeing.
When asked about the number of hours worked per week, most surgeons reported working between 51 and 80 hours per week (69.5%) with the largest group working 61 to 70 hours per week (29.0%).
Another matter of contention within the specialty is the potential workforce shortage, which is believed to be a result of factors such as aging surgeons, surgeon retirement, and a diminished cardiothoracic surgical trainee pool.
The current survey showed an increase in the average age of practicing surgeons by 2 years compared with the 2014 survey (56 years vs. 54 years, respectively). This suggests that a retirement surge is imminent, as is an expected decline in the workforce—from 4,000 surgeons in 2010 to less than 2,900 by 2035, as calculated by another study.
At the same time, with the general population also aging, the anticipated case load will increase from approximately 530,000 cases in 2010 to more than 850,000 cases in 2035, resulting in a 121% increase in case load per surgeon. The good news is that even though jobs are sometimes difficult to find, the current survey showed that 59.2% of practices are looking to hire a new surgeon within the next 2 years, up from 52.3% in 2014.
Also important to note and related to the aging workforce is the growing concern over surgeon performance, especially considering that cardiothoracic surgery is one of the most technically, cognitively, and physically demanding fields.
“Cardiothoracic surgery—as a ‘frontline’ surgical specialty—is at great risk for burnout and depression.”
The survey revealed that 85.3% of cardiothoracic surgeons worked in institutions that did not conduct cognitive and psychomotor performance testing for surgeons who are 65 years or older. This issue, especially with more institutions expected to offer testing programs in the coming years, could potentially contribute to the diminishing cardiothoracic surgery workforce.
Other challenges within the specialty include the rapid introduction of novel technologies and techniques, as well as the pressure to incorporate minimally invasive treatment strategies into practice. The survey showed that while many surgeons have continued to expand their skill sets, approximately half (48.7%) have not learned a new surgical skill in the past year.
In addition, 59.6% of all surgeons reported using a less invasive approach while performing “20% or less” of cardiac surgery cases. For general thoracic surgery, 28.5% of surgeons said they use a less invasive approach “81% or more” of the time.
“It is important that all physicians embrace new technologies and make them a part of their practice,” said Dr. Ikonomidis. “Adopting new surgical techniques and medical treatment methods prevents physicians from becoming obsolete.”
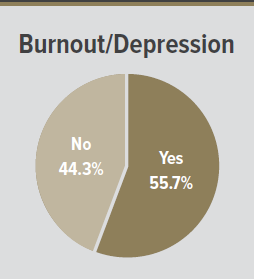
Cardiothoracic surgeons are at great risk for developing burnout symptoms.
Perhaps one of the biggest issues, though, is the risk of depression and burnout within the specialty. More than 55% of surgeons reported symptoms of burnout and/or depression related to their jobs over the past year, which is 10% to 20% higher than that observed in other specialties.
“Cardiothoracic surgery—as a ‘frontline’ surgical specialty—is at great risk for burnout and depression,” said Dr. Ikonomidis. “Surgeons must be honest with themselves regarding symptoms and take steps to prevent burnout and depression.”
This survey did not track specific elements contributing to these symptoms, but Dr. Ikonomidis explained that the “time-consuming, often counter-intuitive, and frustrating” implementation of electronic medical records, as well as increased scrutiny on surgeon productivity and outcomes, are among the factors that likely have impacted the personal wellbeing and emotional health of cardiothoracic surgeons.
The delicate dance of balancing the demands of both professional and personal lives also may influence the risk of depression and burnout. The survey revealed that “work-life balance” is the most common reason for advising against a career in cardiothoracic surgery, with 65.2% of surgeons citing this as “very important.”
“Cardiothoracic surgery is not an ‘elective’ specialty. Patients are sick and need operations now, so a surgeon is not able to choose a convenient time to deliver care,” said Dr. Ikonomidis. “Being a surgeon is a highly stressful occupation and sometimes it is difficult to check your stress at the door when you go home after a hard day’s work.”
Despite numerous external pressures, the practice of cardiothoracic surgery remains strong, according to Dr. Ikonomidis. “It is a vibrant and multidimensional specialty that continues to be practiced at a very high level by an outstanding group of caring, hardworking, and highly intelligent individuals.”
Note: The most recent STS Practice Survey was conducted online from September 16 to November 1, 2019, with results published online in The Annals of Thoracic Surgery on May 14, 2020.