STS News, Fall 2021 — Cardiothoracic surgery training programs represent an increasingly diverse population in the United States, and this can mean more comprehensive care for patients—but faculty and leadership positions need to catch up, according to a study published online in August in The Annals of Thoracic Surgery.
“It is imperative that our workforce represents the diverse patient population we treat,” said senior author Ourania A. Preventza, MD, MBA, from Baylor College of Medicine in Houston, Texas, and a member of the STS Workforce on Diversity and Inclusion. “My thoughts are that diversity and inclusion mean more than gender, race, and ethnicity. They are the first steps toward equity and excellence.”
For this study, Dr. Preventza’s team examined demographic trends among traditional, integrated (I-6), and fast-track (4+3) cardiothoracic surgery programs listed in the Accreditation Council for Graduate Medical Education (ACGME) public database. Using a combination of public resources, the researchers analyzed the characteristics of trainees through July 2020, including their gender and race/ethnicity, as well as any academic appointments bestowed on them.
The researchers found that the proportion of female trainees increased significantly in the past decade, from 19% in 2011 to 24% in 2019. In the area of race/ethnicity, they observed significant increases in underrepresented minority candidates across all types of training programs. From 2019 to 2020, white, Asian, and Hispanic trainees had greater proportional representation in I-6 programs than in traditional curricula, while Black trainees had greater proportional representation in traditional programs.
"It is imperative that our workforce represents the diverse patient population we treat."
While the proportions of women did not significantly differ by training pathway, the overall increase in the proportion of women was attributable to their increased enrollment in I-6 programs. The authors explained that I-6 residency may be more attractive to female medical students than the fellowship track, and they speculated that this may be due to factors including increasingly more women than men entering US medical schools, female residents’ mentorship of medical students, targeted scholarships for women in cardiothoracic surgery, and the appeal of earlier exposure to surgical procedures and research.
“Although the I-6 pathway does not always reduce time spent in training, it may help maximize relevant skills earlier on while enabling greater flexibility for lifestyle choices such as childbearing,” the authors suggested.
Overall, however, interest in cardiothoracic surgery among female medical students remains relatively low, the authors noted, and there is a significant need for same-sex mentors, as well as validation of career compatibility and life goals from both female and male colleagues in the specialty.
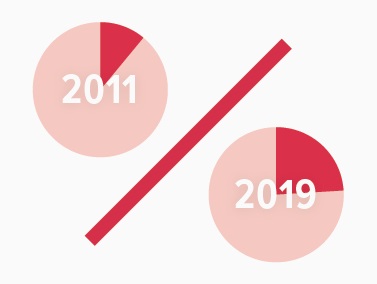
The proportion of female trainees increased significantly in the past decade, from 19% in 2011 to 24% in 2019.
The researchers also observed a low proportion of underrepresented minority trainees who were appointed to faculty positions, noting that this has been the case in previous studies. They posited that with few underrepresented individuals in the pool of eligible candidates, it may take time for diversification to happen in leadership—unless the specialty makes targeted efforts to bring it about. These efforts might mean leadership engagement, a blinded step in candidate evaluation to mitigate bias, structured interviews, equal opportunities to express opinions during rank meetings, and reevaluation of the distribution of appointments and recognitions, the authors advised.
Diversity is an asset to cardiothoracic surgery, explained lead author Jacqueline K. Olive, MD, from Duke University Medical Center in Durham, North Carolina, because diverse backgrounds, experiences, and perspectives enhance patient care—as well as workplace culture and morale. “While statistics on gender, race, and ethnicity provide some metrics for diversity, we should also look beyond these categories to better understand inclusion, and how diverse individuals play a role in clinical and administrative leadership,” said Dr. Olive, also a member of the STS Workforce on Diversity and Inclusion.
“We are no doubt getting better, but we still have a lot of work to do,” said Dr. Preventza. “Our specialty needs to continue to advocate and focus on strategies to mitigate bias in recruitment, retention, promotion, and leadership engagement. The main beneficiary of these efforts will be our patients.”

Dr. Preventza, who recognizes the importance of cultivating a culture in cardiothoracic surgery that encourages diversity, flexibility, and fairness, spent time with trainees at a recent STS Annual Meeting.