STS News, Summer 2021 — The prospect of heart surgery is understandably frightening for patients, but Todd C. Crawford, MD, can tell them from personal experience that it’s worth it.
When he was 19 years old and in pre-med school, Dr. Crawford first began experiencing chest pain. The nurse practitioner at the office where he worked told him that he had a diastolic murmur.
“Of course I knew what the words ‘diastolic’ and ‘murmur’ meant, but until then, I’d been seeing a pediatrician every year for sports physicals, and no one had ever mentioned a heart murmur,” Dr. Crawford said. “I was fortunate to be in the medical community in Kansas City and to know a cardiologist who got me in right away for a stress echo. And sure enough, I had a bicuspid aortic valve with mild insufficiency, and a root aneurysm that was around 4.3 centimeters.”
At the time, Dr. Crawford didn’t pursue aggressive treatment, opting instead to have annual imaging exams to monitor the condition. Fourteen years passed and he remained asymptomatic.
In the meantime, however, a subtle change was occurring, and by the time Dr. Crawford was nearing the end of general surgery residency, the aneurysm was bordering on 5 centimeters.
“But I was too busy to slow down,” Dr. Crawford said. “I got married. My wife and I had a kid. And I hadn’t seen a heart surgeon in years.”
During his first year as a fellow at Penn Medicine’s Division of Cardiovascular Surgery—under the supervision of Joseph E. Bavaria, MD—Dr. Crawford consulted with his colleague and friend Joshua Grimm, MD, who now serves on the Penn faculty. Dr. Grimm advised him to see Dr. Bavaria as a patient.
“Of course Dr. Bavaria is this incredible figure who’s been a leader in aortic surgery, especially aortic valve-sparing root replacements in patients with bicuspid aortic valves,” Dr. Crawford said. “And he also was my boss at the time. I’d done a couple of aortic valve replacements with him earlier in the year, and it was a little intimidating to now see him as a patient.”
Because he thought that his condition had been relatively stable, Dr. Crawford and his wife, Tori, were surprised when Dr. Bavaria advised him to consider surgical repair as soon as possible, saying that he was confident that he could save the aortic valve.
The Crawfords knew Dr. Bavaria’s track record for outstanding surgical outcomes, but any open-heart surgery, especially one involving circulatory arrest and a valve-sparing attempt, is no small consideration. They also worried for their young son, Case, and because both Dr. Crawford and Tori had pre-existing conditions—Tori had undergone a sternotomy 3 years prior for a thymoma—neither was eligible for life insurance.
“The pre-existing condition is a glittering asterisk on your life insurance application,” Dr. Crawford recalled. “We have a 1-year-old, we’re renting a place, Tori’s still working in Baltimore half the month while I’m in Philadelphia. And now we were talking about open-heart surgery.”
With the support of the Penn team and staff at Children’s Hospital of Philadelphia (CHOP) and both Tori’s and Todd’s families, the Crawfords chose to go through with the operation on February 8 of this year. “It happened to be the day after the Super Bowl, and I’m from Kansas City, and my Chiefs were playing,” Dr. Crawford remembered. “And obviously the loss was a tremendous letdown, but it was hard to care too much about that because all I could think about was having heart surgery the next day.”

Dr. Crawford spent several days in the hospital, and then "I was off to the races," he said.
The surgical team admitted Dr. Crawford into the OR early, taking additional precautions to respect his privacy as a surgical fellow at the hospital. Dr. Grimm and the chief cardiac resident, Michael Ibrahim, MD, PhD, visited with the Crawfords before surgery and Dr. Grimm assisted Dr. Bavaria with the operation. Dr. Grimm’s wife, Jessica, even brought Tori lunch during the surgery.
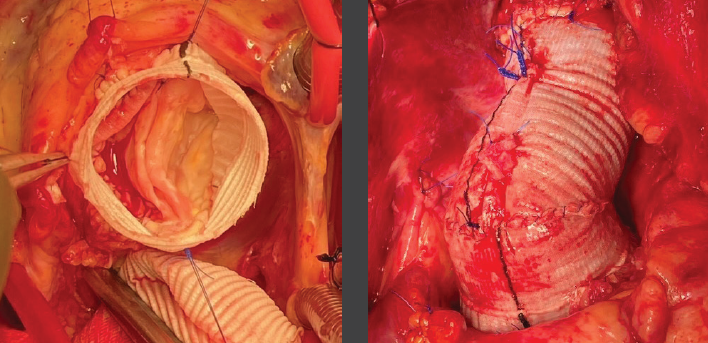
Despite a complex bicuspid aortic valve repair, the valve-sparing root replacement was a complete success; Tori recalls Dr. Bavaria’s phone call to her at the completion of the operation. “We knocked it out of the park,” he said. Now several months after the surgery, Dr. Crawford says, “It was more like a bottom-of- the-ninth walk-off grand slam!”
“Tori was my rock during this whole experience,” Dr. Crawford said. “From our last moment alone before I was wheeled to the OR, to spending every second at my bedside and barely sleeping while I was in the hospital. She was the person who pushed me to ambulate, to eat, to start to recover, and she gave me the strength to get through this challenge and get back to work.”
After 5 weeks, during which Dr. Crawford experienced tachyarrythmias as the irritability of his heart recovered, the CHOP team welcomed him to the OR once again—as an operating surgeon.
“That first week was wild,” Dr. Crawford said. “I only live a mile from the hospital, more or less across a large bridge, and I typically walk to work. But I didn’t want to overdo it the first day by walking so many steps before the workday even began,” he recalled. “But then my Uber canceled on me. I ended up walking the distance so I wouldn’t be late for work. By the time I got there, I’m sure my heart rate was in the 130s.”
The Penn/CHOP team was overwhelmingly compassionate, Dr. Crawford said, and on that first day he worked on a congenital operation. “I think that shows the support of Penn for their trainees,” he said. “To be willing to put me in that situation and be patient with me. From there, I went back to the adult hospital in April, and I was extremely busy, taking overnight call…and my heart’s been great. I feel great. I have great endurance. And now we’re almost 4 months out, and I feel very fortunate.”

Dr. Crawford described his wife, Tori, as his "rock."
Dr. Crawford, now looking toward his second year of fellowship, said that he has a new appreciation for his patients’ apprehensions. In May, he had the opportunity to give back and perform his first valve-sparing root replacement with Wilson Y. Szeto, MD.
“We all try to maintain the same focus with every operation, but there was something extra special about that day and the relationship that followed with that patient,” he said. “Patients appreciate it when I tell them I’ve been through this, and I know it’s rough, but this is what you can expect, and things do get better.”
If you know of a unique member experience that should be featured in STS News, contact stsnews@sts.org.