STS News, Winter 2021 — Nine years after the US Food and Drug Administration (FDA) approved the first transcatheter aortic valve replacement (TAVR) device, TAVR therapy volume is skyrocketing and patient outcomes continue to improve.
TAVR case volumes have risen steadily since 2011 and, in 2019, the state-of-the-art therapy exceeded all forms of surgical aortic valve replacement (SAVR), according to a report using data from the STS/American College of Cardiology (ACC) Transcatheter Valve Therapy (TVT) Registry.
“This report summarizes massive amounts of data about the US TAVR experience and includes 276,316 patients treated from 2011 to 2019,” said John D. Carroll, MD, chair of the STS/ACC TVT Registry Steering Committee and lead author of the report. “In addition to volume, the data document a substantial improvement in quality of care over the last 9 years.”
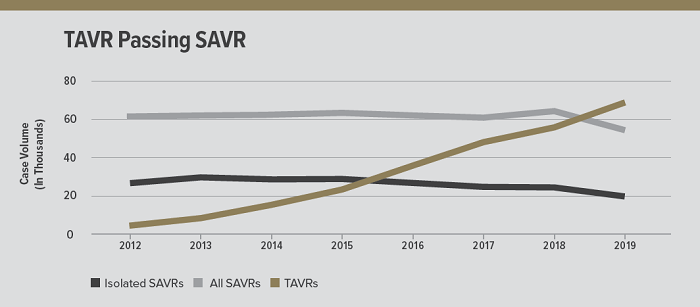
In 2019, TAVR case volume exceeded all forms of SAVR, positioning TAVR as the dominant form of AVR.
Expanded Patient Access
TAVR now is a treatment option for most aortic stenosis patients. In 2011, it was indicated only for those at extreme risk for surgery. In 2012, high-risk patients were added, followed by intermediate-risk patients (2016), and low-risk patients (2019). These risk categories importantly have helped shape clinical trial design and regulatory approval, as well as real-world practice.
The report, published in The Annals of Thoracic Surgery and the ACC journal, showed that from 2011 to 2018, extreme- and high-risk patients remained the largest group undergoing TAVR, but in 2019, intermediate-risk was the leading patient group. It’s worth noting that in the first year of FDA approval for low-risk patients, the TAVR population included 8,395 low-risk patients—a likely contributor to SAVR case volume falling behind TAVR.
When the FDA first approved use in low-risk patients, experts widely predicted that it would pave the way for an even more rapid TAVR expansion, with the transcatheter-based therapy replacing a significant portion of SAVR procedures in the years to come.
Nonetheless, the number of people undergoing any form of AVR—transcatheter or surgical—grew by 94% from 2012 to 2019. This likely is due to greater disease awareness and an aging population, which results in more people being treated.
TAVR Programs Offered in All 50 States
In response to the demand, more and more hospitals are launching TAVR programs. In 2020, Wyoming saw its first site open, extending TAVR’s reach to all 50 states and 730 participating centers. The number of TAVR procedures performed per site varies, but as the number of sites has increased, so has the total annual volume. In 2019, most centers performed an average of 84 TAVR procedures, while 161 sites each performed fewer than 50 cases.
“The TVT Registry allows us to see major trends occurring in the real-world TAVR patient population, including a rapid growth in both the number of hospital sites performing TAVR and case volume as we treat a broader spectrum of patients,” said Dr. Carroll.
Voluntary public reporting for TAVR programs will be available in fall 2021. See page 13 for more information.
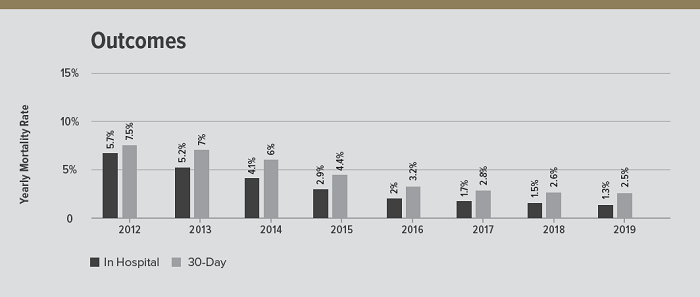
The data on outcomes after TAVR show a substantial improvement in quality of care over the last 9 years.
Outcomes Improve Over Time
While SAVR traditionally has been the standard treatment for severe aortic stenosis, TAVR has emerged as a strong alternative treatment, providing promising patient outcomes.
Since the early days, there has been steady and dramatic improvement in TAVR mortality. In 2012, in-hospital mortality was 5.7%, falling to 1.3% in 2019. The 30-day mortality also decreased—from 7.5% to 2.5% during that same period.
Hospital stays for patients also improved—from 7 days to 2 days. More specifically, low-risk patients had a median length of stay in 2019 of only 1 day—an overnight hospital stay—with some patients discharged the same day. In the early TAVR period, most patients were discharged to another care facility; however in 2019, 90.3% of patients were discharged home, while only 6.6% were discharged to a rehabilitation or extended care facility and 2.5% to a nursing home.
“The transformation of care for patients with aortic stenosis has been dramatic,” said Dr. Carroll.
Two areas in which experts said they want to see improvement are stroke rates and the 30-day pacemaker implantation rate. Although the stroke rates showed a small, downward trend, the in-hospital stroke rate was 1.6% and the 30-day rate was 2.3%. The 30-day pacemaker implantation rate remained relatively unchanged since 2011. The early rate was 10.9%, it peaked in 2015 at 15.1%, and then slowly declined to 10.8% in 2019.
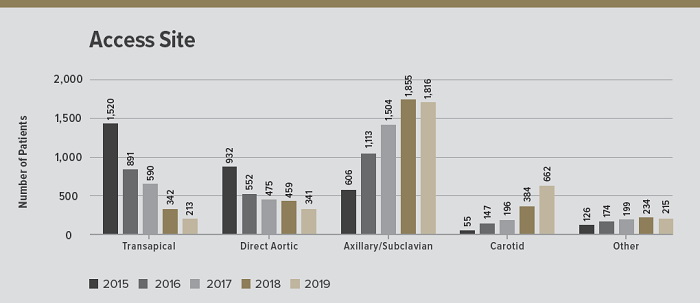
The state of TAVR report documented a clear shift in vascular access.
Patient-Reported Quality of Life
The TVT Registry has been innovative in gathering patient-reported data on quality of life, using a questionnaire tool before treatment. The survey provides a measure of the patient’s perception of his/her health status, including symptoms, impact on physical and social function, and quality of life.
In 2018—the most recent year with 1-year patient-reported outcomes data—80.7% of all patients who were alive 1 year after TAVR, reported a good quality of life. In addition, a subgroup analysis revealed that a favorable outcome was achieved in 77.7% of high-risk patients, 83.6% of intermediate-risk, and 85.8% of low-risk patients.
“The routine use of patient-reported health status using the questionnaire has allowed this new metric to emerge,” said Dr. Carroll. “A better understanding of a patient’s baseline status and the impact of their aortic valve disease is possible. It also provides an assessment of whether the intervention has caused an improvement in the patient’s life.”
Racial Disparities in TAVR
Racial minorities are underrepresented among patients undergoing TAVR in the US, according to the report. For all years, TAVR patients were predominantly white. While the number of black patients receiving TAVR increased from 504 during the early TAVR period to 2,948 in 2019, only 4% of all patients receiving TAVR were black—this has not changed in the past 9+ years.
Possible contributing factors include access to primary care, referral for further testing, and bias at a treatment level, as well as insurance, socioeconomic factors, cultural beliefs, and patient preferences. Researchers said that they expect these gaps to stimulate further research.
“The TVT Registry can monitor whether there are unexpected differences among people of different races, ethnic groups, and rural residency,” said Dr. Carroll. “While it cannot ascertain causes, the Registry can assess whether there are changes associated with variables such as expansion in the number of sites, campaigns to alter disease awareness, and other mechanisms to reduce disparities in care.”
COVID-19 Challenge
And finally, the COVID-19 pandemic has had an impact on all programs, but especially on those performing TAVR with urgent clinical indications.
The report stated that the coronavirus “impaired submission of data” from some sites in 2020. As a result, researchers expect to see major decreases in the number of patients being treated. The Centers for Medicare & Medicaid Services has already announced that it will not hold hospitals and physicians responsible for meeting volume requirements mandated for reimbursement for a range of procedures, including TAVR.
According to the researchers, "further growth is expected with recovery of the health care system" after COVID-19.
The report, “STS-ACC TVT Registry of Transcatheter Aortic Valve Replacement,” is available at annalsthoracicsurgery.org.