STS 2022 DAY 1 — In today’s STS 2022 session, “It’s Not in the Books…So How Do They Do It?”, faculty will present artful approaches and clinical outcomes for congenital heart repair operations, including bicuspidization for truncal valve repair and 3-year results for right ventricular tract reconstruction with a valve created from the right atrial appendage (RAA).
Yves d’Udekem, MD, PhD, from Children’s National Hospital in Washington, DC, will describe a case involving a 2-year-old girl with severe right ventricular to pulmonary artery conduit stenosis and truncal valve regurgitation. The girl’s truncal valve and truncus arteriosus had previously been repaired with a femoral vein homograft when she was 9 days old.
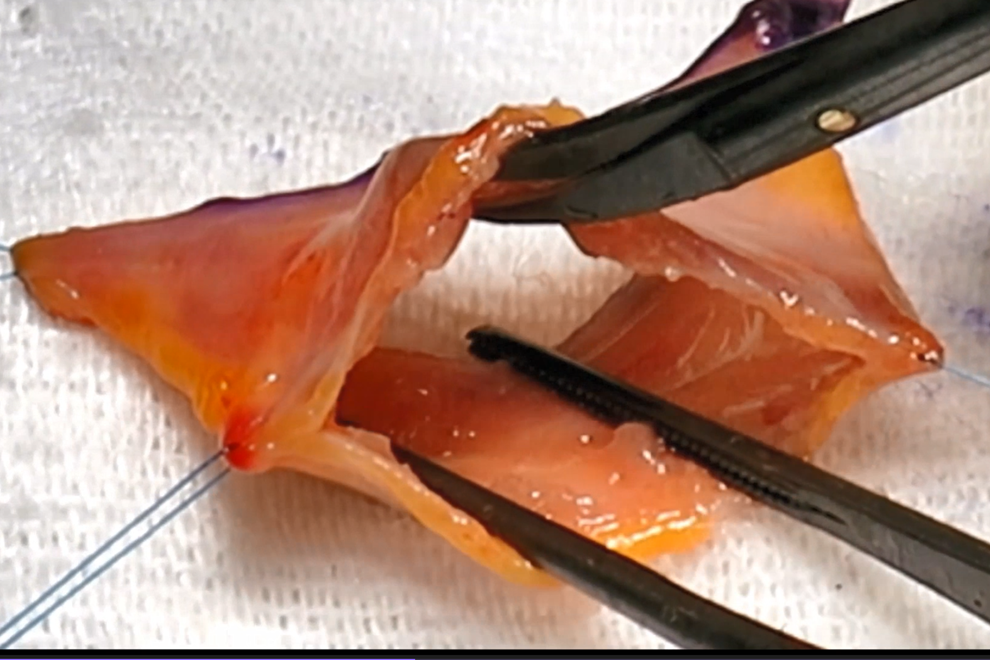
During subsequent operation, the surgical team made the decision to create a bicuspid valve, dissecting dysplastic tissue, closing the gap between the zones of apposition between both right and left cusps, and reducing the root with a triangular resection of the anterior sinus.
Attendees will hear the history, the rationale, and the step-by-step process the team used to implement this successful procedure. “Paradoxically, reducing the size of the aorto-ventricular junction increases leaflet mobility and decreases postoperative gradient,” noted the abstract authors.
Also featured in the session are findings in 68 patients whose native pulmonary valves were absent, atretic, or irreparably stenotic and underwent repair with a valve—created intraoperatively from the RAA—to correct right ventricular outflow tract dysfunction. Ahmad Ali Amirghofran, MD, from the Shiraz University of Medical Sciences in Iran, will describe outcomes of these operations from 2018 to the present.
“The procedure is reproducible and can effectively prevent pulmonary insufficiency, at least in the mid-term period, and may delay or even omit the need for future pulmonary valve replacements,” the researchers observed. They found that while the approach was applied mostly in patients with tetralogy of Fallot, it also demonstrated promise in patients with pulmonary atresia, truncus arteriosus, absent pulmonary valve syndrome, and other conditions.
These abstracts are just two among the fascinating presentations in “It’s Not in the Books…So How Do They Do It?”, which begins today at 11:15 a.m. ET. Other abstracts will explore risk factors in cone repair for Ebstein anomaly, creation of a polytetrafluoroethylene valved conduit, and prophylactic commissural resuspension during an unroofing procedure for an anomalous coronary artery.
Registration is still open for STS 2022, now an all-virtual experience, at sts.org/annualmeeting.